Altitude Sickness: Understanding, Symptoms, Prevention & Treatment
Published On : 26th Sep, 2025 By Himalayan Dream Team

Altitude Sickness: Symptoms, Prevention & Treatment for Trekking in Nepal
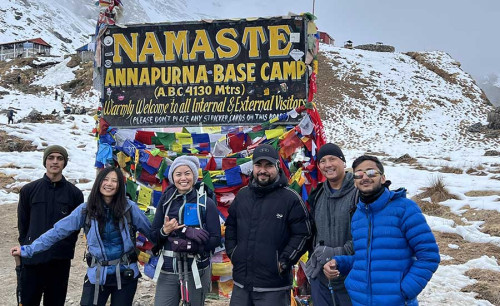
Altitude sickness—commonly known as acute mountain sickness (AMS)—is one of the biggest challenges faced by trekkers and climbers around the world. Whether you are preparing for the Everest Base Camp Trek, the Annapurna Circuit, or high-altitude expeditions in the Andes or Rockies, understanding altitude sickness is essential for both your safety and enjoyment.
At Himalayan Dream Team, we believe that knowledge and preparation are the keys to a successful adventure. This comprehensive guide explains what altitude sickness is, its symptoms, prevention methods, treatment options, and specific tips for trekking in Nepal’s Himalayas.
What is Altitude Sickness?
Altitude sickness occurs when your body cannot adapt to the reduced oxygen availability at higher elevations. Although the percentage of oxygen in the atmosphere remains constant at around 21%, the air pressure decreases with altitude, meaning fewer oxygen molecules are available with each breath.
Most trekkers begin to feel symptoms at 2,500 meters (8,200 ft), and the risks increase significantly above 3,000 meters (9,800 ft).
Types of Altitude Sickness
There are three main stages of altitude-related illness, each with increasing severity:
1. Acute Mountain Sickness (AMS)
-
Mildest and most common form
-
Feels similar to a hangover
-
Symptoms: headache, nausea, dizziness, fatigue, loss of appetite, mild shortness of breath
2. High Altitude Pulmonary Edema (HAPE)
-
Severe, life-threatening condition where fluid builds up in the lungs
-
Symptoms: breathlessness at rest, persistent cough (sometimes frothy sputum), chest tightness, extreme fatigue, blue lips/fingertips
-
Requires immediate descent and medical attention
3. High Altitude Cerebral Edema (HACE)
-
Critical emergency where fluid accumulates in the brain
-
Symptoms: severe headache, confusion, loss of coordination (ataxia), hallucinations, seizures, coma
-
Can be fatal if untreated—immediate evacuation is necessary
Symptoms of Altitude Sickness
Recognizing symptoms early is the most important factor in preventing life-threatening complications:
-
Headache (most common first sign)
-
Nausea and vomiting
-
Loss of appetite
-
Difficulty sleeping
-
Fatigue and weakness
-
Dizziness and lightheadedness
-
Swelling of hands, feet, or face (in some cases)
If ignored, mild AMS can quickly develop into HAPE or HACE.
Who is at Risk of Altitude Sickness?
Altitude sickness can affect anyone, regardless of age, gender, or fitness level. However, certain factors increase the risk:
-
First-time high-altitude trekkers
-
Rapid ascent without acclimatization
-
Pre-existing respiratory or heart conditions
-
History of AMS in previous treks
-
Overexertion or dehydration
-
Children and older adults
How to Prevent Altitude Sickness
1. Ascend Gradually
-
Follow the golden rule: “Climb high, sleep low.”
-
Do not increase your sleeping altitude by more than 500m per day once above 3,000m.
2. Include Acclimatization Days
-
Essential in treks like Everest Base Camp (rest in Namche Bazaar & Dingboche) or Annapurna Circuit (rest in Manang).
-
Go for short acclimatization hikes to higher ground and return to sleep lower.
3. Stay Hydrated & Eat Well
-
Drink 3–5 liters of water daily.
-
Avoid alcohol and excess caffeine.
-
Eat a high-carbohydrate diet for steady energy.
4. Train Before Your Trek
-
Cardio and endurance training strengthen your lungs and stamina.
-
Practice hiking with a backpack for better preparation.
5. Medication
-
Acetazolamide (Diamox): Helps speed acclimatization.
-
Dexamethasone: For severe AMS prevention and treatment (prescription only).
-
Always consult your doctor before taking medication.
6. Listen to Your Body
-
Never ignore early symptoms.
-
If symptoms worsen—stop ascending immediately.
Treatment of Altitude Sickness
-
Mild AMS: Rest, hydrate, and avoid further ascent.
-
Moderate AMS: Use Diamox or supplemental oxygen; take a rest day.
-
Severe AMS, HAPE, or HACE: Immediate descent of at least 500m, oxygen therapy, and medical evacuation if needed.
In Nepal, helicopter evacuation is available in emergencies, especially from high-altitude trekking routes like EBC, Gokyo, and Annapurna. Himalayan Dream Team always includes safety protocols for clients.
Altitude Sickness & Trekking in Nepal
Nepal’s popular treks often cross high passes above 5,000 meters, such as:
These elevations make altitude awareness critical. Our guides are trained in first aid and AMS response, ensuring trekkers are safe at every stage.
Myths About Altitude Sickness
-
❌ “Only unfit people get AMS.” → Wrong. Even elite athletes can suffer.
-
❌ “Diamox cures altitude sickness.” → It helps prevent, not cure severe stages.
-
❌ “You can push through it.” → Ignoring symptoms is dangerous.
-
❌ “Drinking alcohol warms you up.” → Alcohol worsens dehydration and AMS risk.
Why Altitude Sickness is Common in Nepal Treks
Nepal’s trekking trails are unique because they ascend rapidly to very high altitudes within a short timeframe. Popular routes often push trekkers above 3,000–5,000 meters, where the risk of altitude sickness is highest.
Everest Base Camp Trek (5,364m)

Altitude sickness in Nepal treks is most frequently experienced on the Everest Base Camp Trek, especially after Namche Bazaar (3,440m) when oxygen levels start to drop. The rapid altitude gain between Namche, Tengboche, Dingboche, and Lobuche makes acclimatization essential. At Himalayan Dream Team, we include carefully placed rest days in Namche and Dingboche, short acclimatization hikes to places like Everest View Hotel and Nangkartsang Hill, and continuous health monitoring from our guides to reduce the risk of altitude sickness and ensure a safe journey to Everest Base Camp.
Annapurna Circuit Trek (5,416m at Thorong La)

Another classic adventure where altitude sickness in Nepal treks becomes a real concern is the Annapurna Circuit Trek, especially when approaching Thorong La Pass (5,416m). The trail climbs steadily from the lush valleys to alpine landscapes and thin-air high passes, making proper acclimatization in Manang and Pisang vital. Himalayan Dream Team designs the Annapurna Circuit itinerary with extra days in Manang for side hikes to Gangapurna Lake or Ice Lake, giving trekkers the best chance to adapt naturally and cross Thorong La safely without severe altitude sickness.
Manaslu & Tsum Valley Treks (5,160m at Larkya La)

For remote and less crowded adventures, altitude sickness in Nepal treks often occurs on the Manaslu Circuit and Tsum Valley Treks, which reach Larkya La Pass at 5,160m. The remoteness of the region and limited rescue facilities mean prevention and early action are critical. Himalayan Dream Team ensures trekkers are supported with expert guides trained in AMS management, strategically paced itineraries, and the option of horse or emergency evacuation support when needed. With our guidance, trekkers experience Manaslu’s pristine landscapes without altitude sickness disrupting their once-in-a-lifetime journey.
👉 This is why careful itinerary planning with rest days is essential to prevent AMS in Nepal.
How the Human Body Adapts to High Altitude
The body undergoes several changes when exposed to thinner air. Understanding these adaptations helps trekkers respect their limits:
-
Increased Breathing Rate: More frequent breaths supply extra oxygen.
-
Higher Heart Rate: Circulates oxygen faster to vital organs.
-
Red Blood Cell Production: Body creates more red cells to carry oxygen.
-
Blood Flow Changes: Prioritizes brain, lungs, and heart over muscles.
⚠️ These adaptations take time—hence gradual ascent and acclimatization days are crucial.
Altitude Sickness in Children and Older Adults
Children and seniors can successfully trek in Nepal, but they are often more sensitive to altitude changes.
Risks for Children:
-
Difficulty expressing early symptoms like dizziness or nausea.
-
Higher likelihood of dehydration.
-
Need for slower pace and frequent breaks.
Risks for Seniors:
-
Pre-existing conditions (heart, lungs, blood pressure).
-
Slower acclimatization capacity.
-
Medication side effects at altitude.
👉 With careful monitoring, gentle pacing, and proper rest, both groups can trek safely in the Himalayas.
Packing Essentials to Prevent Altitude Sickness
Carrying the right gear helps prevent and manage AMS effectively. Essential items include:
-
Hydration Gear: Reusable bottles, water purification tablets/filters, hydration salts.
-
Medical Supplies: Diamox (if prescribed), pain relievers, anti-nausea tablets, blister kits.
-
Nutrition: Energy bars, nuts, dried fruits, chocolates.
-
Clothing: Warm layered outfits, gloves, hats, moisture-wicking base layers.
-
Other Equipment: Trekking poles, sunglasses, sunscreen, sleeping bag rated for cold temperatures.
💡 Tip: Pack light but smart—your safety kit is as important as your trekking boots.
Helicopter Evacuation in the Himalayas: What You Should Know
In Nepal, helicopter rescue is the fastest option during severe altitude sickness cases (HAPE or HACE).
-
Where rescues are common: Gorakshep, Gokyo, Dingboche, Manang, Thorong Phedi.
-
Average response time: 1–3 hours depending on weather.
-
Cost: Can range from USD 3,000–6,000 (covered by insurance if pre-approved).
-
Requirement: Travel insurance must include emergency helicopter evacuation.
👉 At Himalayan Dream Team, we help clients coordinate with insurance companies and arrange safe evacuation if needed.
First Aid Kit Checklist for High-Altitude Treks
A personal first aid kit is a must-have on Himalayan treks. Here’s what to include:
-
Altitude Medication: Acetazolamide (Diamox), Dexamethasone (emergency use).
-
Pain & Fever Relief: Ibuprofen, Paracetamol.
-
Stomach Care: Anti-diarrheal (Loperamide), oral rehydration salts.
-
Infection Control: Broad-spectrum antibiotics (doctor prescribed).
-
Wound Care: Bandages, blister patches, antiseptic cream.
-
Other Tools: Pulse oximeter, thermometer, lip balm, hand sanitizer.
✔️ Guides from Himalayan Dream Team carry group medical kits, but having a personal kit adds extra safety.
Altitude Sickness vs. Food Poisoning: How to Tell the Difference
Some symptoms of altitude sickness and food poisoning overlap, but recognizing the differences can save your trek.
Altitude Sickness Symptoms:
-
Headache and dizziness
-
Shortness of breath, especially at night
-
Nausea without diarrhea
-
Worsens with altitude gain
Food Poisoning Symptoms:
-
Stomach cramps and diarrhea
-
Vomiting soon after meals
-
Often linked to poorly cooked meat or unfiltered water
-
Improves within 24–48 hours with rest and hydration
👉 If unsure, never ascend further until symptoms are gone.
The Role of Sherpa Guides in Managing AMS

Sherpa guides are not only expert navigators but also first responders in case of altitude sickness.
-
Monitoring Trekkers: They notice early signs of AMS that trekkers may ignore.
-
Adjusting Itineraries: Guides may recommend an unscheduled rest day.
-
Emergency Support: They coordinate oxygen use, horse transport, or helicopter evacuation.
-
Local Remedies: Sherpas also share traditional practices like garlic soup or herbal teas that help with acclimatization.
🌟 With Himalayan Dream Team, our trained Sherpa guides ensure trekkers have both cultural insight and medical safety on every trek.
Frequently Asked Questions (FAQs)
1. What are the 3 stages of altitude sickness?
AMS (mild), HAPE (lung fluid buildup), HACE (brain swelling).
2. Can you get altitude sickness at 2,000 feet (600m)?
Unlikely. Most cases occur above 2,500m.
3. Can you get altitude sickness on a plane?
Commercial aircraft are pressurized, so AMS is rare, but some may feel mild discomfort.
4. What supplements help prevent AMS?
Ginkgo biloba and iron (for anemia patients) may help, but evidence is limited.
5. How to prevent altitude sickness naturally?
Gradual ascent, hydration, nutrition, and acclimatization are the safest methods.
6. Can altitude sickness occur after returning home?
Yes, in rare cases, delayed symptoms can occur but usually resolve quickly.
7. What is the best altitude sickness prevention medication?
Acetazolamide (Diamox) is most commonly prescribed.
8. Can children get altitude sickness?
Yes. Children are equally susceptible and require careful monitoring.
9. How do trekkers in Nepal manage AMS?
By following acclimatization schedules, trekking with experienced guides, and using evacuation support if needed.
10. Is altitude sickness fatal?
If untreated, HAPE and HACE can be fatal. Early detection and descent save lives.
Final Thoughts – Trek Safely with Himalayan Dream Team
Altitude sickness is a real challenge, but it doesn’t have to stop you from experiencing the majesty of the Himalayas. With the right preparation, acclimatization days, and guidance, most trekkers complete their journeys safely.
At Himalayan Dream Team, our experienced Sherpa guides, carefully designed itineraries, and emergency support ensure that your trek is not only adventurous but also safe. Remember: in the Himalayas, slow and steady wins the summit.
Recent Posts

18th Jan, 2026

11th Jan, 2026

28th Dec, 2025

2nd Dec, 2025

24th Nov, 2025

21st Nov, 2025

10th Nov, 2025